WA liver cancer scheme launched
 A new liver cancer project, first of its kind in WA, will apply the latest techniques to analyse patient tumours and test new treatments.
A new liver cancer project, first of its kind in WA, will apply the latest techniques to analyse patient tumours and test new treatments.
Primary liver cancer is where a malignant cancer starts in the liver. It is responsible for the third-most cancer related deaths worldwide, behind only lung and stomach cancer.
Rates of the most common form of primary liver cancers have been increasing steadily in Australia by 4-5 per cent per year for the past three decades.
Average survival after diagnosis is only 12 months and patients often present at an advanced stage when treatment options are limited.
A new research project will be carried out through a new $10.8 million research centre made possible by a $5 million Cancer Research Trust grant and $5.8 million from Minderoo Foundation, Curtin University, The University of Western Australia, Harry Perkins Institute of Medical Research, the State Government and charitable organisations.
Professor Peter Leedman says the research would be a true collaboration of medical specialists, experts in liver disease and cancer researchers.
“It will establish a process, where patient samples are analysed and tested with a range of potential treatments,” he said.
“Interestingly, the diagnosis of primary liver cancer has typically been made with a blood test and an MRI, but not with a biopsy.
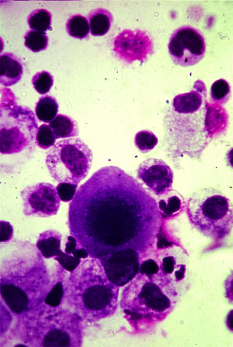
“We now have the latest advanced genomics technology in Perth that can analyse a liver tumour biopsy at the single cell level and look at each tumour’s molecular fingerprint and individual pathology as well as compare a patient’s early and late stage cancer.
“By defining the underlying biology of each tumour, we will be able to provide more precision in treatment selection, eventually matching the ‘right patient to the right drug’ but we also expect to uncover new pathways that can be attacked with new drugs,” Professor Leedman said.
Some patient tissue will undergo advanced genomics analysis by UWA Professor Alistair Forrest at the Harry Perkins Institute while Curtin University will use patient tissue to grow organoids, or mini livers.
Associate Professor Nina Tirnitz-Parker said the new project aimed to improve outcomes for people with primary liver cancer.
“We can establish organoids, miniaturised versions of an organ, from patient tumour samples that will be profiled,” Associate Professor Tirnitz-Parker said.
“We will also establish a repository of organoids that represent different tumour subtypes and then perform drug screenings and make informed decisions on the best possible treatment choices without any side effects to the patient.”
The team aims to develop a unique large resource of approximately 500 liver cancer samples over five years from across Australia, which on a global scale is a sizeable collection.
“Most importantly, the project will make a difference to the treatment of liver cancer and contribute to greater international understanding of the disease,” she said.







 Print
Print